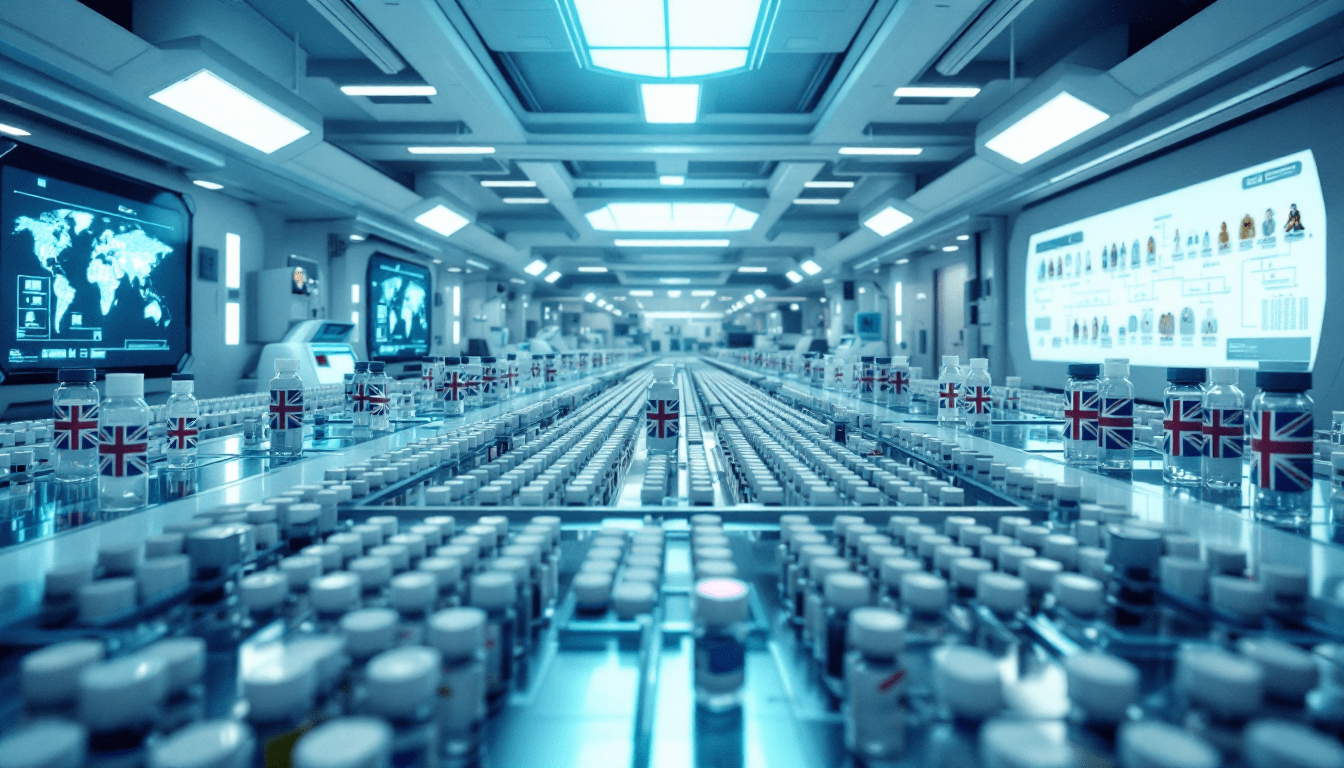
Could We 23AndMe An Entire Nation?
What if every person in Britain had their DNA analysed? A bold proposal examines the logistics, costs, and timeline for genotyping an entire nation - from mail-out spit kits to massive lab automation. The ultimate genetic census could be closer than you think.