The Horrifying Reality Of "Trans" Surgical Butchery
NSFW: Sexual "reassignment" surgery has been pursued as a radical experiment on human bodies. Early procedures were characterised by anatomical amputation, functional destruction, and crude morphological approximation. No true reconstruction was achieved, only surgical illusion.

Physicians traditionally uphold the Hippocratic principle, “first, do no harm.” In the United States, contemporary adaptations of the oath reflect evolving values. In the United Kingdom, doctors adhere to the General Medical Council’s guidelines rather than a sworn oath. In Thailand, Hippocratic principles merge with Buddhist ethics, emphasising compassion and social duty.
During the Weimar Republic, homosexual doctor Magnus Hirschfeld emerged as a pioneering researcher in sex and gender. In 1930, under his supervision, Lili Elbe underwent one of the earliest documented gender reassignments, which included orchiectomy (testicle removal) and penectomy (penis removal); he died following a failed uterine transplant. Hirschfeld’s work influenced Dr. Harry Benjamin in New York, who later advanced hormonal interventions. In 1933, the Nazi regime destroyed Hirschfeld’s Institute for Sexual Science, forcing his exile.
In addition to psychiatrists for therapy, he had hired Ludwig Levy-Lenz, a gynecologist. Together, with surgeon Erwin Gohrbandt, they performed male-to-female surgery called Genitalumwandlung—literally, “transformation of genitals.” This occurred in stages: castration, penectomy and vaginoplasty. (Scientific American's glowing praise for a Dachau doctor.)
Alex Coppen has documented the origins of this macabre trade in exhaustive detail. From Baron Ferdinand von Reitzenstein and Eugene Steinach's bizarre experiments, to Einar Wegener, Arno Ebel, and how Hirschield's colleagues like Erwin Gohrbandt ended up involved in the Dachau Hypothermia Experiments.
As Scientific American was forced to note this was indeed a "twist," as murder often is:
Levy-Lenz, who like Hirschfeld was Jewish, fled Germany. But in a dark twist, his collaborator Gohrbandt, with whom he had performed supportive operations, joined the Luftwaffe as chief medical adviser and later contributed to grim experiments in the Dachau concentration camp.
Harold Gillies, a New Zealand-born plastic surgeon, revolutionized reconstructive techniques during both World Wars. In 1946, he performed a phalloplasty on Michael Dillon, applying principles refined in post war trauma surgery.
Much of this pales in comparison to the horrors inflicted on David Reimer by psychologist John Money, documented in the 2000 book "As Nature Made Him: The Boy Who Was Raised as a Girl."
Reported success rates from the 1980s (68–86%) rely on short-term, subjective outcomes rather than objective long-term data. There are no standardised guidelines for assessing surgical success; instead, outcomes are measured almost entirely by patient self-reports. Unsurprisingly, patients who have already undergone irreversible procedures tend to affirm them as “successful.” This absence of objective benchmarks allows World Professional Association for Transgender Health (WPATH) and surgeons to present such surgeries as effective without rigorous evidence, creating a misleading picture of safety and efficacy.
Many surgeons performing SRS operate from private clinics in Thailand, where medical negligence laws are far weaker than in the West. This legal vacuum allows surgeons to advertise globally and profit from vulnerable patients while evading accountability. WPATH, while presenting itself as an authority, does not establish enforceable standards or accept responsibility for outcomes.
By endorsing these procedures internationally without oversight, WPATH effectively legitimises a medical tourism industry which prioritises profit over patient safety.
Compounding the issue, several prominent WPATH members are themselves transsexuals, such as Dr. Marci Bowers. While this may confer personal insight, it also raises questions about conflicts of interest. Those who have undergone or actively perform SRS may face implicit pressure, psychological, ideological, or professional, to advocate for these procedures, potentially at the expense of objective medical evaluation. When the same community which defines “standards of care” includes practitioners with personal or financial stakes in the continuation of high-risk, experimental surgeries, the oversight of patient safety becomes further compromised.
Many patients now fear reporting complications due to potential blacklisting by surgeons. Online communities (e.g. Reddit) actively suppress discussion of adverse outcomes; criticism is often met with censorship, removal of posts or bans.
No one, especially those suffering from mental illness. deserves to be treated this way. These surgeries are so experimental patients turn up to A&E with horrific complications doctors and nurses have absolutely no clue how to help. Males with faux vaginas turn up to gynaecologist appointments expecting the doctor to know how to treat a hollowed-out borehole in their rectum leaking faecal fluid the patient mistakes for normal discharge.
Unlike appendectomy or hip replacement, technique varies widely among surgeons. Most vaginoplasty involves penile disassembly and inversion to form a cavity. Phalloplasty often uses grafted tissue from the arm or thigh to construct a non-functional phallus devoid of erectile capacity.
The medical community’s departure from evidenced-based restraint represents a breach of fundamental ethical obligations. Patient well-being has been subordinate to ideological conformity.
Vaginoplasty for Male-to-Female Subjects
Modern genital reconstruction originates in early 20th-century gynecological experimentation. In 1904, James Baldwin documented neo-vagina creation via intestinal transplant for vaginal agenesis. The first confirmed "transsexual" vaginoplasty was performed on Dora Richter in 1931 at Magnus Hirschfeld’s "Institute for Sexual Science" in Berlin, marking a shift from reconstructive correction to elective anatomical reassignment.
The vaginoplasty procedure involves constructing a neo-vagina on a male body. Surgeons use penile and foreskin tissue to form the vaginal opening and reposition the urethra. A skin graft, typically harvested from the penile shaft or abdomen, is used to line a surgically created cavity between the rectum and bladder. This space is packed with gauze post-operatively to encourage graft adherence.
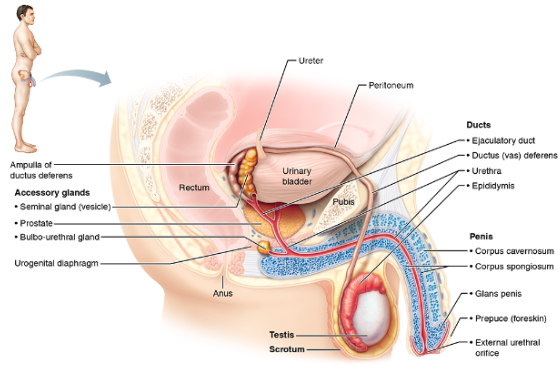
Anatomically, the procedure entails excavating a cavity between the rectum and bladder, which is then lined with inverted penile skin. The vas deferens (sperm delivery tube) is excised, while the urethra is preserved and rerouted. The confined pelvic space presents significant surgical problems, including the body’s persistent attempt to close the non-healing wound and the inherent risk of damage to adjacent bowel and bladder, causing faecal and urinal incontinence.
To maintain patency of the neovaginal canal, patients must perform daily dilation using medical-grade dilators (glass dildos) for multiple hours. This lifelong requirement prevents stenosis but imposes severe lifestyle limitations. Failure to adhere to dilation protocols results in canal closure, graft failure, and complications such as fissures (tears in the grafted tissue) or strictures (narrowing due to scar contraction).
Strictures can precipitate rectovaginal fistulae, allowing faecal matter to leak into the neovagina. Patients often misattribute this discharge to typical vaginal secretions, interpreting it as “euphoria inducing”.
Complications include persistent post-operative bleeding due to granulation and dehiscence – splitting open or bursting apart of a surgical wound, incision, or organ along natural or surgical lines, and persistent infections. Some patients also report erectile tissue left over, necessitating the need for further revisions.
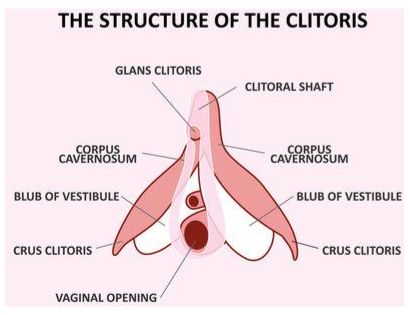
Surgeons fashion a neo-clitoris from the glans, claiming preserved erogenous sensation and orgasmic potential. This assertion contradicts established neurobiology.
The female clitoris is a complex organ with extensive internal structure and thousands of nerve endings integrated into a broader neuro-endocrine system. Stimulation triggers oxytocin release, initiating uterine and pelvic contractions, a process physiologically impossible in male anatomy due to the absence of corresponding structures.
Claims of “nerve hookup” or reinnervation enabling female-type orgasm are anatomically fraudulent. The neo-clitoris comprises transposed penile nerve endings lacking the structural or hormonal context for female sexual response (figure 2). Online stories of “full-body orgasms” are psychogenic artifacts, not physiological outcomes. Additionally, patients report their "clitoris" falling off due to necrosis, causing uncontrollable urine spraying.
A frequent complication is ingrown hair within the neovaginal canal. Despite preoperative electrolysis, hair follicles remain in grafted skin. Upon inversion, these hairs grow inward, forming abscesses or discharging through the neovaginal opening. Patients often report expelling hair, necrotic tissue, and faecal matter, phenomena misinterpreted as vaginal self-cleaning.
Vulvoplasty uses scrotal and penile skin to construct external genitalia, labia majora, labia minora, and urethral opening. This procedure may be performed with or without vaginoplasty. While vulvoplasty alone carries lower morbidity, most patients opt for combined surgery to achieve a more complete aesthetic approximation, often motivated by a desire for penetrative intercourse.
WPATH-endorsed materials claim vulvoplasty permits orgasm via clitoral stimulation equivalent to vaginoplasty. This is scientifically impossible. The neo-clitoris, fashioned from the glans penis, lacks the anatomical substrate for female orgasmic response.
Orchiectomy and Penectomy
Orchiectomy involves the surgical removal of both testes, eliminating the primary endogenous source of testosterone. Testosterone, produced by Leydig cells, regulates male reproductive development and secondary sexual characteristics.
Castration results in drastic hormonal reduction, causing loss of libido, muscle mass, bone density, and other androgen-dependent traits. These effects are well-documented in men undergoing androgen-deprivation therapy for prostate cancer, where testicular removal or chemical castration produces the same outcomes. It is therefore highly likely identical consequences occur in individuals undergoing orchiectomy for SRS, making WPATH’s assurances of preserved vitality and function misleading at best and deceptive at worst.
Penectomy entails the amputation of the penis, with removal of associated structures such as the vas deferens and often the prostate. Some patients opt for penectomy and orchiectomy only without any creation of the neo-vagina structures, most because they are so dysmorphic and unhappy with their body they cannot dream of having intercourse with another.
Some opt to keep their prostate so they can still enjoy anal sex, some keep their vaginal opening (NSFW) and some keep their testicles in a jar, and some receive ball implants (NSFW). Some even opt for phalloplasty and clitoral expansion also known as “metoidioplasty”, which sees the natal female clitoris expanded to resemble a micropenis.
Physiologically, male sexual response is inextricably linked to reproductive function. Ejaculation involves the expulsion of semen, a mixture of sperm and accessory gland secretions, through coordinated muscular contractions.
Female orgasm is a neuroendocrine event centered on clitoral stimulation and pelvic muscle activity without gamete release. These processes are biologically distinct and non-interchangeable, despite claims by WPATH and SRS surgeons, and the trans community via their online boasts of “full body orgasms”.
Sigmoid Vaginoplasty and its Consequences
In cases where penile tissue is insufficient, often due to prior puberty blockade (puberty blockers) surgeons may use segments of bowel, typically sigmoid colon, to construct a neo-vagina.
Intestinal epithelium is simple columnar, secreting mucus and facilitating absorption. While this provides moisture, the tissue is histologically and functionally incongruent with vaginal mucosa, which is stratified squamous and non-keratinised. Patients take to the internet to discuss sigmoid vaginoplasty and the ability to enjoy “rough sex” afterwards.
The consequences of using bowel tissue are severe and predictable. The neo-vagina emits a permanent faecal odour. The epithelial lining remains metabolically active, absorbing secretions and potentially introducing pathogens into the peritoneal cavity.
Patients report discharge of mucus, necrotic tissue, and blood, often misinterpreting these as signs of “vaginal health”.
Case Analysis: Iatrogenic Damage in Youth Transition
The case of Jazz Jennings illustrates the catastrophic outcomes of paediatric medical transition. Administered puberty blockers at age 10, he experienced arrested genital development, resulting in a microphallus which precluded standard penile-inversion vaginoplasty.
He subsequently underwent sigmoid vaginoplasty, suffering numerous complications including wound dehiscence and stenosis, necessitating multiple surgical revisions, all shown live on TV. This saw rooms full of adult doctors telling him how to dilate his new neo-vagina, with his mother implying if he did not keep up with the dilation schedule at university, she would force the dildo up there herself.
Jennings was "transitioned" by his parents at age five when he proudly proclaimed to his mother he was a girl and enjoyed wearing girls dresses and shoes. This prompted his mother to get him on puberty blockers at 10, causing the micro-penis and failure of the “usual” SRS surgery.
His public statements, such as “I still do not feel like myself”, indicate persistent psychological distress and possible regret following irreversible mutilation. Magazines often interview 16 year old Jennings about his ability, or inability to orgasm due to the puberty blockers.
Jennings’ surgery was performed by two big names in the medical world; Dr Marci Bowers and Dr Jess Ting.
Despite having two of the best surgeons Jennings also experienced several post-operative complications as horrifically detailed in several YouTube videos. Much like other SRS patients, Jennings underwent up to four surgeries to create his neo-vagina; not unusual at all with some patients receiving up to eleven.
Phalloplasty: Structural/Functional Limitations
In 1946, Gillies’ five-stage phalloplasty rolled abdominal tissue into a tube to form a urethra, wrapped it with skin to create a penis, connected it to the natural urethra, shaped the base, and sculpted the tip into a glans.
This method laid the foundation for modern phalloplasty.
Later refinements, including free flaps, nerve anastomosis, and microsurgery, improved urination, sensation, and cosmetic outcomes while reducing complications. The procedure cannot replicate erectile function due to the absence of corpus cavernosum.
As a result, there are devices they can wrap around their “phallo” to harden it, or erectile devices. Imagine a pump inflated before intercourse, which is stored in the testicles. However, this pump is often rejected and forcefully expelled by the body and can increase the chances of the phalloplasty failing.
Complications which seem never ending include, urinating blood, bladder spasms, immune system failure, persistent urinary odour, urinary spraying, fistulas, and necrosis (skin death).
Much like the “female orgasm lie”, female to male phalloplasty patients do not achieve orgasm, despite claims by surgeons and patients. This is due to not having a prostate, as male orgasm is produced through coordinated contractions of the prostate, seminal vesicles, and pelvic floor muscles that expel semen and generate the orgasmic sensation.
In allotransplantation cases, lifelong immunosuppression is necessary, introducing risks of renal toxicity, hypertension, opportunistic infection, and malignancy. Graft rejection can result in necrosis and complete loss of the neo-phallus. Patients have reported waking up and finding their artificially-grafted penis next to them in bed, instead of attached to them, due to necrosis.
Additionally, arm grafts experience loss of sensation, extreme swelling and nerve pain, and often necrosis. Often, thigh grafts will be used instead, which experience the same complications. Despite receiving their phalloplasty patients still report dysphoria and regrets. One bonus of using arm/thigh grafts is patients can transfer tattoos from arm to penis.
A documented psychological phenomenon involves patients attributing maternal attachment to the phallo graft, treating it as an externalised object of care, or “their baby”. This occurs despite their oestrogen being blocked and replaced with exogenous testosterone, suggesting deep-seated psychological conflicts unaddressed by surgical intervention.
Medical Abandonment of Ethics
Genital reassignment surgery is a radical, experimental practice which violates fundamental biological and ethical principles. It destroys healthy tissue to create non-functional simulacra, ignores profound physiological constraints, and exacerbates rather than alleviates psychological distress.
The above procedures are affectionately termed “bottom surgeries” by the transsexual community, presumably to make them more appealing to children and teenagers, and to hide to true extent of the invasive surgical procedures.
Accurate descriptors include: orchectomy (testicle removal), penectomy (penis amputation), vulvoplasty, and vaginoplasty. Most patients require multiple revision surgeries to address complications.
The medical establishment’s adherence to ideologically-driven misinformation represents a gross violation of anatomical truth and clinical ethics.
The medical establishment has suppressed honest discussion regarding catastrophic outcomes, prioritising ideological conformity over patient safety. These procedures are not reconstructive; they are iatrogenic mutilations which sterilise, disfigure, and often psychologically cripple vulnerable individuals.
It represents a profound ethical and medical failure. The claim a surgically-altered male can experience "female orgasm" is not only scientifically false, but a cruel deception which preys on vulnerable individuals suffering from mental illness. This is not the first time doctors have collectively been caught in the middle of horrific behaviour.
From both a Christian and medical ethics perspective, it constitutes a complete betrayal of the Hippocratic Oath, prioritising irreversible, experimental mutilation over genuine healing. In a word, it is evil.