The NHS: A Sacred Cow Beyond Saving?
In the summer of 2023, my girlfriend was diagnosed with appendicitis. For the next two and a half months she was at the mercy of the National Health Service. These are my thoughts on Britain’s sacred cow.

In the summer of 2023, my girlfriend was diagnosed with appendicitis. For the next two and a half months she was at the mercy of the National Health Service. These are my thoughts on Britain’s sacred cow.


Abolish the Lords. Relocate Parliament to the geographic centre. Bind all nations through one lower house. Let each control local application through separate upper houses. End devolution's chaos. Build a constitutional structure capable of absorbing a hundred territories without amendment.
Christ's radical call to forgive enemies disrupts humanity's revenge cycles. At Calvary, God absorbed judgment to create mercy, breaking evil's perpetuation. As England fractures, the path forward requires absorbing anger without returning it—we cannot lose who we are on the altar of wrath.
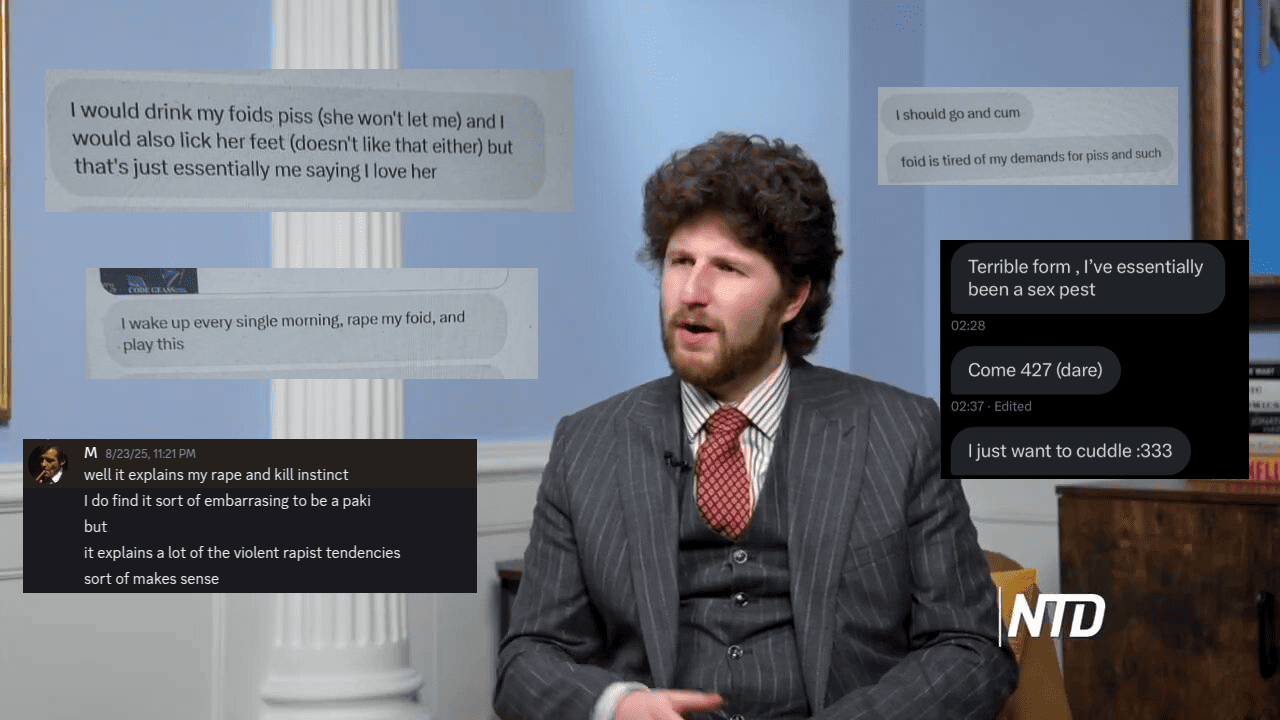
A Restorationist writer published her own story dealing with my co-editor. One of many which are emerging with similar details. After a vicious pre-emptive smear campaign portraying myself and others as suffering a "psychopathic episode," we forwarded what we found to the police.
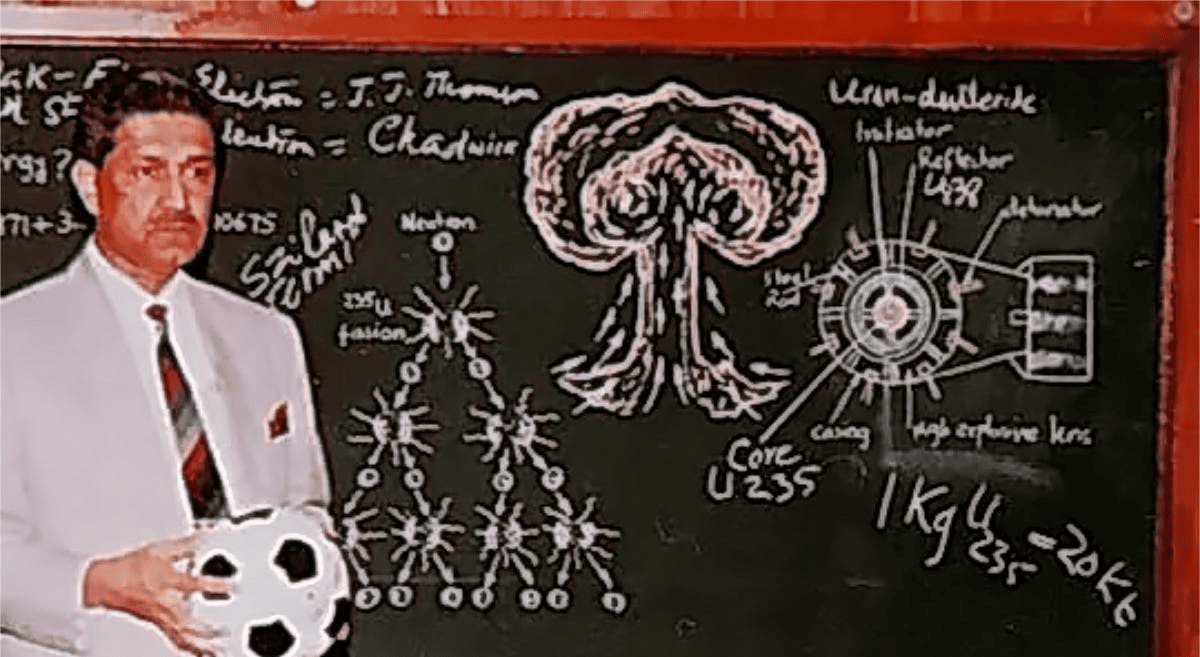
A metallurgist stole nuclear secrets from Europe, then sold atomic weapons capability like a franchise—complete with manuals, components, and customer support. His clients? Iran, Libya, North Korea. The bombs he helped build are still out there. One man nearly broke the world. A true Bond villain.