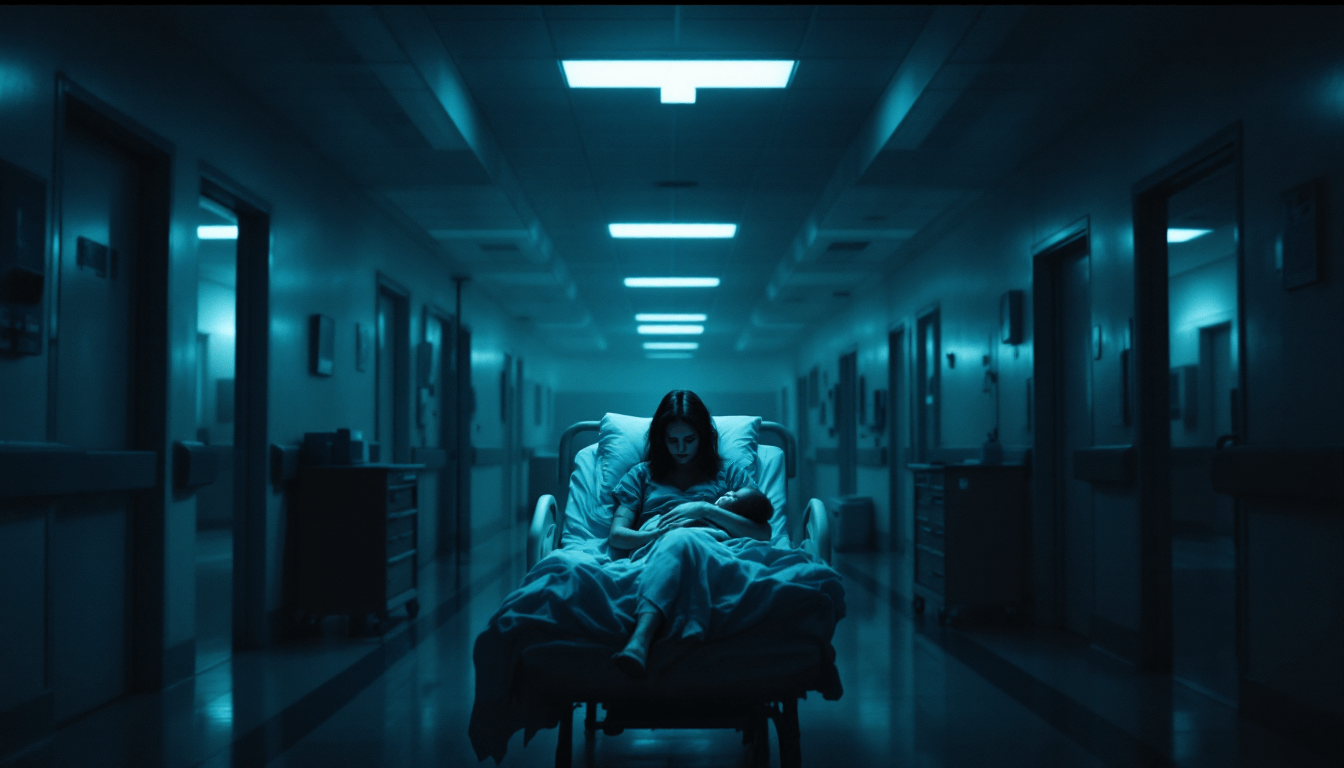
Two Births, Two Traumas: Just Another Day On The NHS
A mother's harrowing account of two traumatic NHS births marked by dismissed concerns, unnecessary medical complications, cruel staff treatment, and institutional neglect. Both deliveries involved back-to-back babies, emergency procedures, and emotional abuse from midwives.